While Lucy Goodson, a third-year resident at the University of Washington Department of Emergency Medicine, was working during the region’s historic heatwave in June, the hospital’s patients were sitting in the hallways, trying to find a place to stay cool.
At the time, the influx of patients left the hospital without an empty bed or available nurse. Although some of these patients had already been treated for heat-related illnesses, they could not be sent home, because they had nowhere safe to go.
“Even if we got [patients] cool we couldn’t send them home. What were you going to do to send someone back to a house that’s 110 degrees?” She said. “There was a limit, and unfortunately, we were at it.”
Months after a historic heatwave rocked the pacific northwest, doctors and health officials are still reflecting on how the deadliest weather event in state history overran the Seattle area medical system. Top health officials and climate scientists gathered, Aug. 26, to discuss the impact of the three-day weather event.
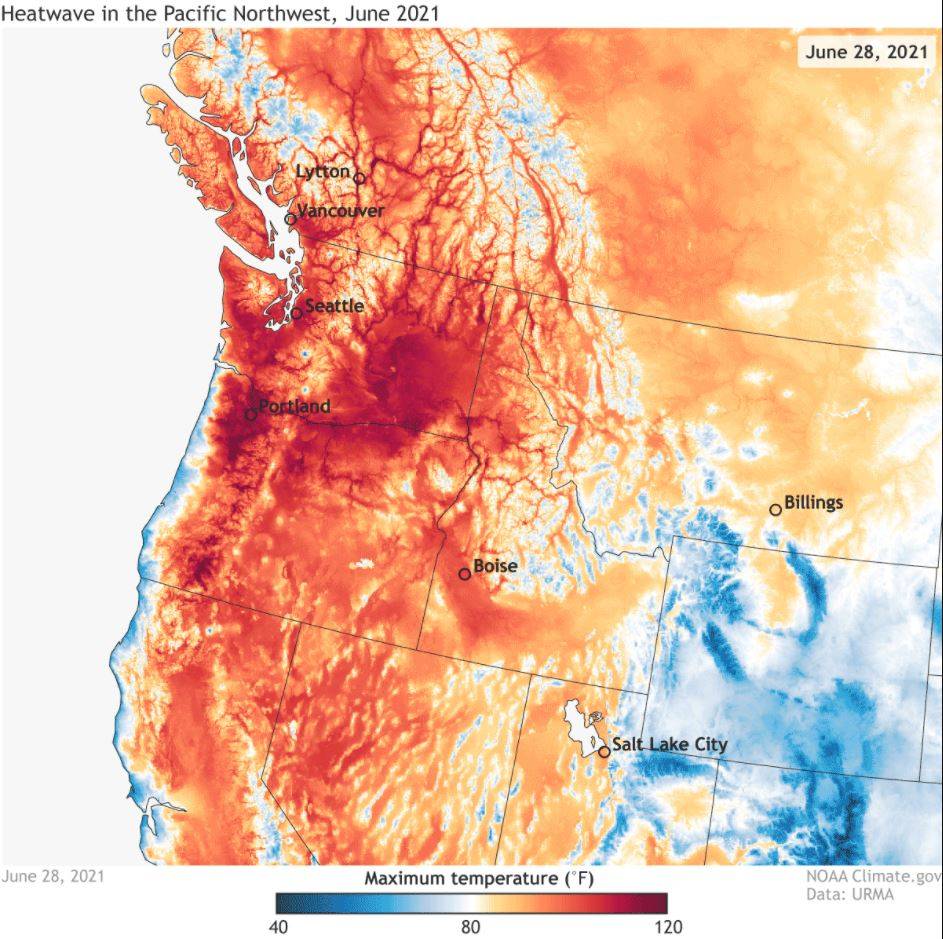
The heatwave, lasting from June 26-28, brought some of the hottest temperatures the state has ever experienced. During the stretch, Seattle recorded its first, second and fourth hottest day in history. Nationwide, it was the hottest June in recorded history.
“That heatwave was virtually impossible without climate change,” said Kristie Ebi, a professor at the University of Washington Center for Health and the Global Environment.
The heatwave was responsible for 1,350 deaths, including 500 in Washington. Health officials expect that number to rise as counting continues.
Ebi said 35% or more of worldwide heat-related deaths can be attributed to human-caused climate change. Climate change is also responsible for an increase in the frequency and intensity of extreme heat.
Cameron Buck, the director of the Valley Medical Center in Renton, said over the three days his hospital saw a 13% to 15% increase in patient volume.
During an eight-hour peak period, Buck said the hospital was seeing a new heat-related patient every nine minutes. This came at a time when the hospital’s 30 ICU beds were already operating between 90 to 95% of capacity.
“While we thought we were somewhat prepared, that eight-hour period of time completely overwhelmed the community hospital,” Buck said.
Jeremy Hess, a professor and director of the Center for Health and the Global Environment at the University of Washington, said the availability of hospital beds has been something the state medical system has been dealing with for a long time. He said although the region has grown rapidly, the medical system has not kept pace.
He said if there is a 20% increase in patients over an 18-month span in Washington the hospital system will be taxed. If that 20% occurs over six months, the system will run out of beds.
“We don’t have any slack in the system, and that was going into the event,” he said. “COVID made it that much worse.”
Although COVID-19 hospitalization rates were low in June compared to today’s numbers, county hospitals were still burdened by the pandemic.
“Fortunately [the heatwave] was near one of our nadir’s for COVID illness in our hospital,” said Steven Mitchell, medical director at Harborview Medical Center in Seattle. “I just shudder to think what it would be like today.”
During the event, Mitchel said all regional hospitals were in bad shape, while some were in severe shape. He said the Valley Medical Center was down to one ventilator, while other hospitals were running on generators, at risk of losing power and facing evacuation.
“We have a completely new frame of reference,” Mitchell said. “It has taught us some invaluable but painful lessons.”